
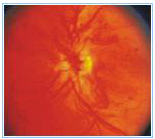
Diabetes affects the retina and this condition is called as diabetic retinopathy. It is a micro angiopathy affecting the retinal blood vessels. The main features of diabetic retinopathy are micro vascular (small blood vessel) occlusion and leakage. As a result of this, there is reduced blood supply to the retina .Due to leaking blood vessels, hemorrhages and fluid accumulation in the retina can occur.
This initial stage is also called as Non-Proliferative Diabetic Retinopathy (NPDR).
As a result of reduced blood supply to the eye because of diabetes the eye will start forming its own new blood vessels Proliferative Diabetic Retinopathy (PDR), which are fragile hence they can rupture and bleed any time which lead to sudden drop in vision. This is known as Vitreous hemorrhage. Sometimes in more severe forms traction on retina can develop that can lead to retinal detachment.
This requires treatment in the form of laser to the eye or surgery or both.
The treatment is to stabilize the patient's vision and prevent further progression of visual loss.
Fundus Fluorescein Angiography (FFA) and Optical Coherence Tomography (OCT) are the two investigative procedures which may be done before the treatment plan for Diabetic Retinopathy.
This is a diagnostic procedure where in fluorescein dye is injected into a vein of the hand and then a series of photographs of the patient's retina are taken. This gives us a picture of the passage of the dye through the microvasculature of the eye. This helps us to know the status of the blood vessels in retina and reveals blockage, excess leakage of the dye in case of abnormal new blood vessels. It also helps us to know whether the patient needs laser photocoagulation or not.
The treatment is usually in the form of laser or rarely an injection is given in the eye. The laser treatment may be done in 1- 3 sittings.
Every patient once diagnosed to have diabetes should have regular eye check ups every 6 months.